by Ben Best
Most of the unreferenced material on this webpage comes from information in the book THE PROMISE OF SLEEP by William C. Dement, MD, PhD. Dr. Dement has devoted his life to sleep research from the time he was a medical student in the 1950s, and is widely regarded as being the world's foremost authority on the subject of sleep.
This article is concerned with the nature of sleep and the impact of sleep upon health. This article is not much concerned with the impact of health conditions upon sleep, although I will give a brief overview of the subject in the next section.
People having sleep disturbances due to health conditions may find some useful hints in this article, but they should look elsewhere for detailed information, diagnosis & treatment. Health conditions leading to sleep disturbances are often not recognized by physicians or misdiagnosed. Such conditions are much more apparent in a sleep clinic than they are in a physician's office where the patient is fully awake.
Insomnia is a symptom, not a disease condition itself, although it can indicate a disease condition. Someone extremely worried or excited about events in their life can experience insomnia without suffering from a health condition.
The most common and worrisome medical condition that disturbs sleep is sleep apnea. Snoring is a sign of impaired breathing associated with partial closure of the throat, a condition which can increase with age due to decreasing muscle tension, with obesity as a significant contributing factor. As the condition worsens it leads to complete closure of the throat. The apnea victim suffers temporary suffocation, often for as long as a minute, becomes aroused enough to regain breathing and then falls into deeper sleep. The cycle often repeats many hundreds of times per night without the victim being aware of the condition other than experiencing the effects of sleep deprivation. The victim may adapt to chronic fatigue and sleepiness as being "normal". Automobile accidents, high blood pressure, heart attacks and stroke which are primarily due to sleep apnea are usually wrongly attributed to other causes. Approximately one-quarter of men and about the same proportion of post-menopausal women have some degree of sleep apnea. Not sleeping on one's back can help — some people sew a ping-pong ball onto the back of their pajamas. Mechanical devices or surgery may be the only way to correct the problem.
Some sleep disturbances are regarded as common problems of childhood. An estimated 7% of 9-year-olds occasionally wet their beds. About 15% of children sleepwalk at least once.
Nocturia is defined as interruption of sleep at least twice nightly due to a need to urinate — a common cause of sleep loss among older adults. A 2003 National Sleep Foundation survey found that 65% of respondents between 55 and 84 years of age reported having nocturia at least a few nights per week. (For more information on nocturia, see SLEEPTIONARY/Nocturia.)
Victims of narcolepsy can suffer extreme attacks of daytime sleepiness associated with muscle weakness, often in response to strong emotions. Persistent insomnia is often due to restless leg syndrome, gastroesophageal reflux, fibromyalgia, depression, arthritis or other medical conditions. Menstruation, pregnancy, and "hot flashes" associated with menopause can also disturb sleep.
Although more than half of all people over age 65 experience sleep problems, these disturbances are more often due to medical problems and medication use than due to aging itself [SLEEP; Foley,DJ; 22(Suppl 2):S366-S372 (1999)]. Epidemiological studies indicate that sleeping in excess of 7.5 hours per night is associated with increased mortality, but self-reported sleep-time may simply be time in bed, not actual sleeping [SLEEP MEDICINE REVIEWS; Youngsteadt,SD; 8(3):159-174 (2004)]. Healthy middle-aged volunteers under age 55 were healthier (more resistant to infection) if they slept more than 8 hours per night [ARCHIVES OF INTERNAL MEDICINE; Cohen,S; 169(1):62-67 (2009)].
For more information on sleep disorders, see the American Sleep Apnea Association, the Wikipedia Sleep Disorder page, the Restless Legs Syndrome Foundation and the American Academy of Sleep Medicine websites.
|
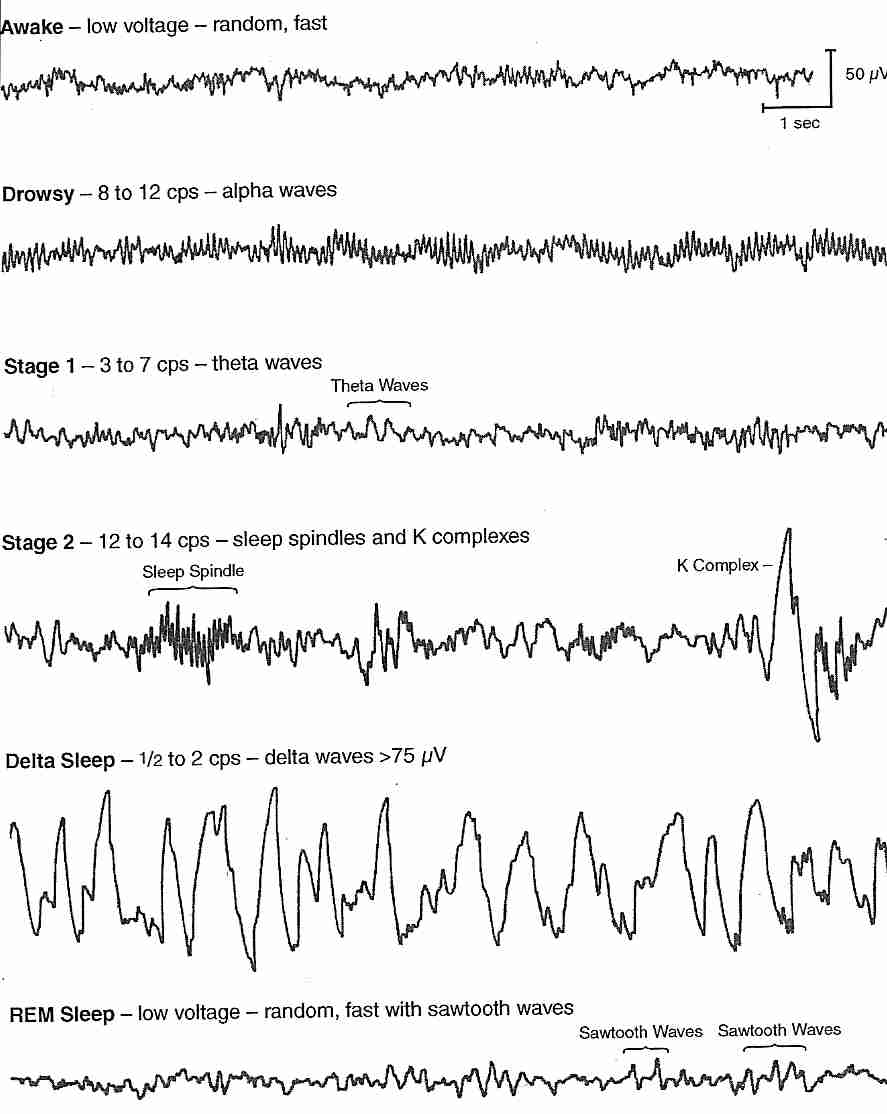
ElectroEncephaloGraph (EEG) recordings of brain waves have defined stages of sleep since the 1950s. In an awakened state a "normal" person's EEG waves are low voltage (small vertical deviation), random and fast (many waves per time period or length of EEG chart). In calm wakefulness with eyes closed the waves become slower (lower frequency — 8 to 10 cycles per second, cps) and are designated alpha waves. The first, very light stage of sleep is called stage 1, characterized by waves that are even slower (3 to 6 cps) which are designated theta waves. Within about 5 minutes the sleeper progresses from stage 1 to stage 2, which is characterized by a theta-wave background punctuated by bursts of high-frequency sleep spindles and high voltage K-complexes. After another 5 or 10 minutes the sleeper enters deep sleep (stages 3 & 4, also known as Slow Wave Sleep, SWS) characterized by very high voltage, low frequency delta waves.
After about an hour the sleeper develops a sleeping EEG pattern that is very similar to the waking-state EEG associated with so-called Rapid Eye Movement Sleep (REM Sleep) in which the eyes move under the eyelids. A young adult's first REM sleep will last about ten minutes before re-entry into deep sleep. Cycles of REM-sleep and NREM (Non-REM) sleep continue through a typical 8-hour sleep, with REM-sleep periods becoming progressively longer. A young adult will typically spend 25% of the sleeping period in REM sleep, whereas older adults have less REM sleep. Infants (who typically sleep 16 hours per day) spend about 50% of sleeping time in REM sleep. Near-term fetuses spend 60% to 80% of their sleep time in REM sleep.
Wakefulness, REM sleep and NREM sleep have been described as three distinct states of consciousness. Both REM and NREM sleep probably perform essential functions for brain maintenance because 24-hour wakeful vigilance would seem more conducive to survival. Deprivation of NREM sleep results in far more sleepiness than deprivation of REM sleep. Yet REM sleep must also perform an important function because people deprived of REM sleep, but not NREM sleep, will enter REM sleep almost immediately upon falling asleep rather than after an hour of NREM sleep, as normally happens. REM sleep is usually, but not always, associated with dreaming. People who demonstrate so-called "lucid dreaming" — ie, consciousness of being in a dreaming condition — invariably have their lucid dreams during REM sleep. Voluntary muscles are typically paralyzed during REM sleep, which may protect against dangerous acting-out of dream content. Normal people — even infants — usually have genital tumescence during REM sleep — which is usually not associated with erotic dreams.
Extended periods of REM sleep are only seen in mammals. Dolphins sleep half-a-brain at at time. The short bursts of REM sleep seen in birds do not last much longer than one second. Reptiles and fish do not exhibit REM sleep. The sleep-like behavior of "lower animals" is mainly a resting condition.
Adenosine TriPhosphate (ATP) provides the brain with energy, but with increasing wakefulness, adenosine without phosphate accumulates, causing sleepiness. Caffeine blocks adenosine action, reducing sleepiness while also impeding learning and memory [BEHAVIORAL BRAIN RESEARCH; 193:79 (2008)]. Sleepiness — the craving for sleep — can be compared to hunger and thirst. There is a general correlation between the time since last eating, drinking or sleeping and the amount of hunger, thirst or sleepiness. After a certain period of time without sustenance the demands of depravation can become increasingly intense, but these demands can come-and-go. Moments of increasingly distracting discomfort occur with increasing frequency and intensity as the period of depravation increases.
Both missing large amounts of sleep in a single night and missing small amounts of sleep over many nights can produce and equivalent amount of sleepiness, sleep deprivation or "sleep debt". Even when the degradation of cognitive and physical performance are the same for both forms of deprivation, the subject is more conscious of the sleepiness or deprivation from a single episode. A study of 48 healthy adults (ages 21−38) subjected to either total sleep deprivation for 2 nights or to chronic sleep deprivation of less than 6 hours per night for 14 days showed comparable cognitive performance deficits in the two groups, but only the first group reported intense feelings of sleepiness [SLEEP; Van Dongen,HP; 26(2):117-126 (2003)]. A psychological adaptation to sleep debt occurs when it accumulates in an incremental fashion over a more extended period — which makes it more dangerous. Most people have a chronic sleep debt without being aware of it. They have adapted, and believe that they are experiencing normalcy. Mood is more worsened by sleep debt than performance, with sleep-deprived people being more negative, depressed & irritable while experiencing less enjoyment of life. Sleep deprivation has been shown to affect risky behavior by decreasing avoidance of losses and increasing seeking of gains [JOURNAL OF NEUROSCIENCE; Venkatraman,v; 31(10:3712-3718 (2011)].
A Gallop poll indicated that nearly a third of respondents remember falling asleep while driving an automobile. People often have "microsleeps" without being aware of them. Automobile accidents due to such incidents are typically unexplained or attributed to other causes. Clearly people with sleep debt can be a danger to others as well as themselves. In an anonymous survey at a San Francisco hospital over 40% of respondents admitted to killing at least one patient due to a fatigue-related mistake.
Dr. Dement discovered a means of objectively quantifying sleepiness (accumulated sleep debt) by observing how long it would take a normal person to fall asleep when lying down with eyes closed in a quiet dark room. People who fell asleep in less than 5 minutes had high levels of sleepiness, whereas people who fell asleep in 15-20 minutes were minimally sleepy. People who remained awake after 20 minutes were awake and alert. (Obviously these measures would not apply to a person in a state of worried emotional distress over a personal crisis.) Dr. Dement found that the ability of his subjects to predict their likelihood of falling asleep was terrible — and he doesn't hesitate to warn of the consequences of people misjudging their capacity for falling asleep at the wheel of an automobile.
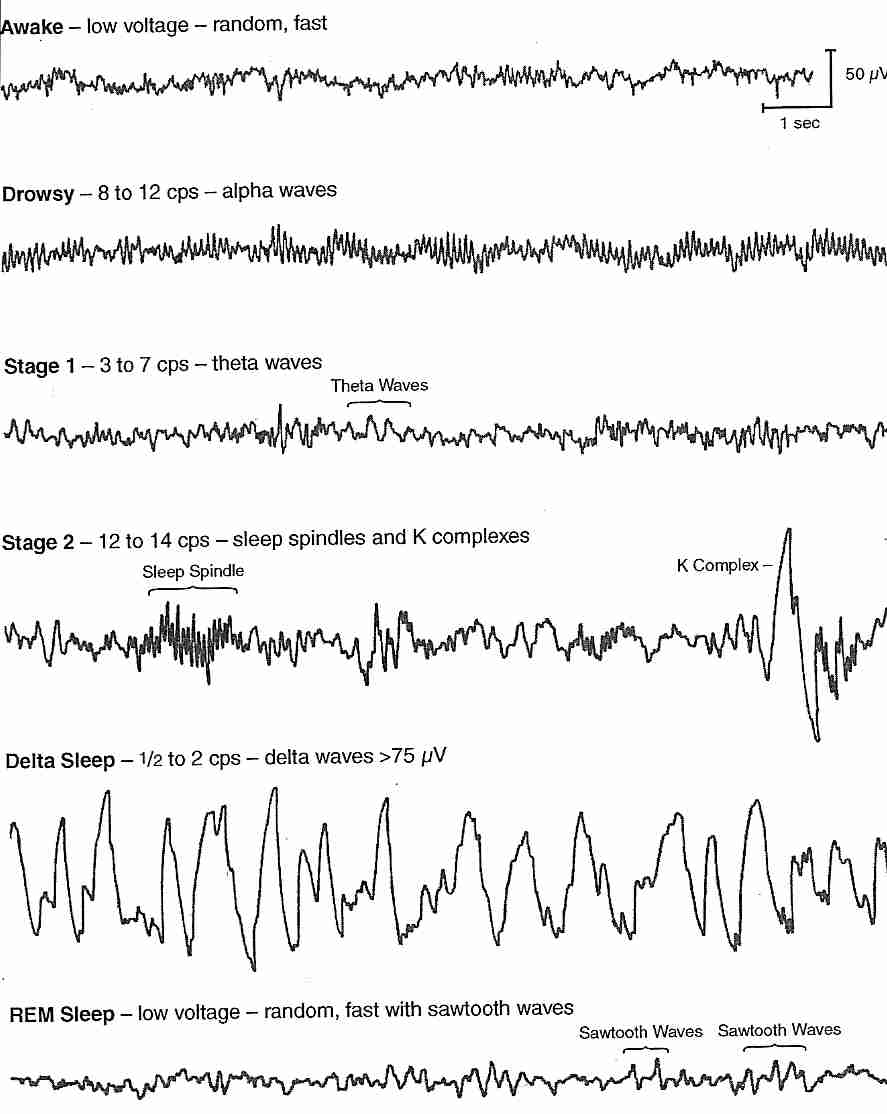
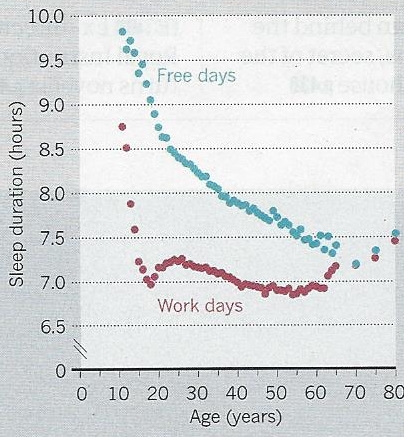
Normal adult volunteers allowed to sleep as much as they wanted (and denied any "distractions") typically slept 12-16 hours per day initially and between 7.5 to 9 hours per night after about three weeks — an indication that most people have chronic sleep debt. Just before puberty children need about 10 hours of sleep per night, whereas teenagers need about 9.5 hours. Children usually get the sleep they need, whereas teenagers are far more likely to be sleep-deprived.
A CONSUMER REPORTS survey reported that more than one quarter of respondents took 30 minutes or more to fall asleep, and one quarter awakened in the night and couldn't go back to sleep for at least a half-hour [CONSUMER REPORTS; 73(9):12-15 (2008)].
About half of people between ages 18 and 29 report daytime sleepiness compared to about a third of those over age 30. The sleep requirement for those between age 40 and 65 is estimated to be about 7 hours per night, less than that of younger adults. As people become more elderly their sleeping becomes increasingly fragmented to the point where sleep and wakefulness are spread-out over day & night in extreme old age. Elderly people sleep less deeply and are more easily awakened. Hours spent in bed can be a poor indication of hours slept or quality of sleep.
Shift workers typically get two hours less sleep when sleeping during the daytime because of their need or desire to interact with other people. "Counterclockwise" shift changes involving rotations to the previous shift are more disruptive to sleep than "clockwise" changes to subsequent shifts.
The word circadian comes from the Latin roots circa ("around", "near") and dies ("day"). The circadian rhythm is the rhythm set by a "biological clock" that affects alertness by hormone release over a 24-hour period. Circadian "clocks" have been discovered in a wide variety of organisms as diverse as humans and fruit flies. Human subjects isolated from external time-of-day cues usually settle into a 25-hour daily cycle.
The "circadian clock" in mammals is located in the SupraChiasmatic Nucleus (SCN) in the hypothalamus, immediately above the crossing of the optic nerves. Light & darkness also strongly influence the release of melatonin. (The decline in melatonin release with senescence is responsible for some of the decline of circadian signaling associated with aging [NEUROBIOLOGY OF AGING; Munch,M; 26(9):1307-1319 (2005)].) Circadian arousal and sleep-inducing signals from the SCN can be hormonal and/or neural [JOURNAL OF APPLIED PHYSIOLOGY; Dijk,D; 92(2):852-862 (2002)]. A notable hormonal effect is an early morning rise in cortisol [HORMONE RESEARCH; Van Cauter,E; 49(3-4):147-152 (1998)]. The circadian clock also influences metabolism & the timing of food intake. Defects in circadian clock genes increase fat mass accumulation & vulnerability to the metabolic syndrome [SCIENCE; Turek,FW; 308:1043-1045 (2005)].
One of the most surprising effects of the circadian rhythm in humans adapted to waking day and sleeping night is an alerting that occurs in the evening. Circadian alerting causes people to be more drowsy in mid-afternoon than in the evening. The effect is stronger for teenagers than for older adults — which means that teenagers are more inclined to be "night owls" who like to sleep-in in the morning. Jet lag is worsened by adjustments required to the circadian rhythm.
Sleep is believed to be a means by which waste products are removed from the space between brain cells [SCIENCE; Herculano-Houzel,S; 342:316-317 (2013) & SCIENCE; Xie,L; 342:373-377 (2013)]. One of those waste products is amyloid-beta, the protein believed to cause Alzheimer's Disease [NATURE; Costandi,M; 497:S19-S20 (2013)].
Healthy adults restricted to less than 5 hours sleep per night have increased insulin resistance and inflammation, an effect which is substantially greater with circadian disruption [DIABETES; 63:1860 (2014))]. Healthy adults who normally sleep less than 7 hours per night were asked to increase their daily time in bed by one hour. After 40 days the subjects showed substantially greater insulin sensitivity [SLEEP; 38:707 (2015)].
Dr. Dement and his colleague observed 18-year-old Randy Gardner set the Guinness world record for time without sleep in 1965. Randy was shaken when he tried to doze and was encouraged to play basketball to stay awake. Toward the end of his 264 hours (11 days) of being awake, Randy became increasingly alert & enlivened by the worldwide media attention he was receiving. His record has remained unbroken for decades, at least in part because ethics committees will not allow sleep scientists to participate in such an ordeal. Dr. Dement observed that although Randy could become very angry in response to being kept awake — and his faculties were clearly impaired — Randy was never in a state that could be called psychotic. Beliefs that sleep deprivation leads to psychosis were at least partially based on the experiences of people who used amphetamines or other drugs to stay awake. Animal experiments on sleep deprivation show no signs of alteration of behavior other than those which would be expected from tiredness.
Alcohol ingestion prior to bed reduces REM sleep — especially in the first half of the night — resulting in impaired memory for recently-learned procedural tasks [SLEEP; Smith,C; 26(2):185-191 (2003)]. Alcohol and sleepiness interact in a way that is far more dangerous than might be expected. Experiments with twelve healthy men in the 20−26 age range showed that either restriction of sleep to 5 hours or a blood alcohol level roughly equal to the United Kingdom limit for automobile driving nearly tripled the number of lane drifting incidents in the 30−60 minute driving period on a driving simulator. Combining both those levels of alcohol with sleep deprivation again nearly tripled the number of lane drifting incidents above that seen for either the alcohol or sleepiness alone. But the reported sleepiness of those who had the alcohol/sleep-deprivation combination was no greater than what was reported by those who had only been sleep deprived [OCCUPATIONAL AND ENVIRONMENTAL MEDICINE; Horne,JA; 60(9):689-692 (2003)].
At the time of puberty both boys and girls begin producing larger amounts of growth hormone, testosterone, prolactin, FSH (Follicle-Stimulating Hormone) and LH (Leutenizing Hormone), whereas melatonin release declines. Growth hormone is secreted mainly during sleep. Inadequate sleep at puberty can stunt growth, and inappropriate melatonin supplementation can delay puberty.
Depressed patients who miss a night of sleep often feel better due to elevated cortisol, but the benefit is only temporary [AMERICAN JOURNAL OF PSYCHIATRY; Voderholzer,U; 161(8):1404-1410 (2004)].
Sleep deprivation in rats compromises the immune system, allowing bacterial overgrowth to cause fatal septicemia [AMERICAN JOURNAL OF PHYSIOLOGY; Everson,CA; 278(4):R905-R916 (2000)]. Sleep deprivation in rats causes an increase in leukocytosis & inflammatory cytokines, which can be quickly reversed by sleep [AMERICAN JOURNAL OF PHYSIOLOGY; Everson,CA; 289(4):R1054-R0163 (2005)]. In healthy volunteers, sleep deprivation increased the level of pro-inflammatory C-reactive protein in a linear, dose-dependent manner [JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY; Meier-Ewert,HK; 43(4):678-683 (2004)].
Cytokine elevation due to sleep deprivation can facilitate viral entry into cells, an effect that can be alleviated by napping [THE JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY; Shearer,WT; 107(1):165-170 (2001)]. Sleep deprivation in humans has been shown to impair the effectiveness of influenza vaccination [JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION; Spiegel,K; 288(12):1471-1472 (2002)]. Viral infections increase interferon (IFN−α) production. Impaired sleep due to IFN−α can can create a viscious cycle of compromised immune defense and sleep deprivation [CYTOKINE; Spath-Schwalbe,E; 12(5):518-521 (2001)]. Healthy middle-aged volunteers subjected to cold virus were about 3 times more likely to become infected if they slept less than 7 hours per night [ARCHIVES OF INTERNAL MEDICINE; Cohen,S; 169(1):62-67 (2009)].
A study of 12 healthy men in the 20−24 year age range showed that 2 days with 4 hours sleep per night resulted in a 33−45% appetite increase for calorie-dense foods having high carbohydrate content. This change was associated with an 18% decrease in the appetite-suppressing hormone leptin and a 28% increase in the appetite-stimulating hormone ghrelin [ANNALS OF INTERNAL MEDICINE; Spiegel,K; 141(11):846-850 (2004)]. Adults reporting 5-6 hours of sleep per night had twice the incidence of impaired glucose tolerance or type 2 diabetes as those reporting 7-8 hours of sleep [DIABETOLOGIA; Chaput,J; 50(11):2298-2304 (2007)]. Sleep restriction increases serum cortisol while decreasing serum leptin and insulin sensitivity, resulting in increased appetite [ENDOCRINE DEVELOPMENT; Leproult,R; 17:11-21 (2010)]. Overweight middle-aged volunteers subjected to two weeks of sleep deprivation (5.5 of sleep opportunity per night) and calorie restriction lost 55% less fat and 60% more fat-free mass [ANNALS OF INTERNAL MEDICINE; Nedeltcheva,AV; 153(7):435-441 (2010)]. Healthy young men (aged 20-35) subjected to one week of sleep deprivation (5 of sleep opportunity per night) showed an approximate 10% reduction in insulin sensitivity (increase in insulin resistance) [DIABETES; Buxton,OM; 59(9):2126-2133 (2010)]. When sleepiness contributes to overeating, obesity and overweight, it constitutes a health hazard. According to the World Health Organization's 2002 World Health Report a body weight index over 21 kg/m2 is causative of 58% of type 2 diabetes cases, 21% of ischemic heart disease and 8−42% of certain cancers. Short sleep is risk factor for weight gain, insulin resistance and type 2 diabetes.
|
A large epidemiological study found that the diffence between the amount of sleeping that occurred during workdays (or schooldays) and free days ("social jetlag") was greatest in late adolescence, and declined toward age 60. More than two-thirds of the participants experienced at least one hour of "social jetlag", whereas a third of participants experienced more than two houors of "social jetlag" per day [CURRENT BIOLOGY; Roennebert,T; 22(10):939-943 (2012)]. Every hour of "social jetlag" increased the chance of being overweight or obese by one-third [Ibid.]. A trend of increasing "social jetlag" between 2002 and 2010 (amounting to about one hour) has been attributed to contributing to the "obesity epidemic" [Ibid.].
Epidemiological studies often show a U-shaped association between sleep and mortality (cardiovacular mortality and all-cause mortality), with the optimum amount of sleep being 7 or 8 hours. Over a five-year period, a decrease in sleep from the optimum has been associated with increased cardiovascular mortality, whereas an increase in sleep from the optimum has been associated with increased non-cardiovascular mortality [SLEEP; Ferrie,JD; 30(12):1659-1666 (2007)].
In 1960 the average sleep duration in the USA was estimated to be 8.5 hours, but 50 years later sleep duration had dropped 1.5-2 hours per night — which has been seen as contributing to an increase in obesity and diabetes [ENDOCRINE DEVELOPMENT; Leproult,R; 17:11-21 (2010)].
From ancient times dreams have been regarded as prophecies, and there have been persons who specialized in interpreting dreams. Many scientists & artists have been inspired by their own dreams. It is not uncommon for people to have had dreams which have affected major life decisions.
Sigmund Freud's 1905 book THE INTERPRETATION OF DREAMS postulated that dreams are an outlet for repressed, forbidden feelings — and that interpreting dreams provides insights into the subconscious which can facilitate psychotherapy. Although many of Freud's theories have lost scientific credibility, it is still probably true that the study of dreaming can provide insight into the anatomical/physiological basis of mind.
Sleepwalking does not occur during REM sleep because the muscles of posture & movement are in a state of paralysis — there is an absence of muscle tone. If REM sleep is accompanied by vivid, emotional dreams it would be counter-productive and dangerous to physically act-out participation. Occasionally people can begin awakening while still in the paralytic, hallucinating REM state and have a nightmarish experience of terrifying helplessness.
About 50% of infant sleeping is REM, declining to adult levels of 20-25% between the ages of 3 to 5. Although dreaming is mostly associated with REM sleep, NREM "dreaming" is less hallucinatory & visual, and more thought-like & fragmentary. Areas of the brain associated with arousal (thalamus & limbic system) are activated in REM sleep, whereas areas associated with executive function (dorsolateral prefrontal cortex) are deactivated in REM sleep [SEMINARS IN NEUROLOGY; Eiser,AS; 25(1):97-105 (2005)].
Some scientists have come to the conclusion that REM sleep is important for consolidation of procedural learning (learning to tie a shoe), but not declarative learning (learning the name of the capital of Latvia). Adjacent articles in the journal SCIENCE argue for and against the REM memory consolidation hypothesis [SCIENCE 294:1052-1058 versus 294:1058-1063 (2001)]. Sleep initiated with ethyl alcohol has been shown to reduce both REM sleep and procedural learning consolidation [SLEEP 26(2):185-191 (2003)]. All mammals (and perhaps all birds) studied display both non-REM and REM sleep, yet there is no correlation between brain size, learning rate, sleep time or REM sleep between species [SCIENCE; Siegel,JM; 294:1058-1063 (2001)]. Sleep in most mammals is more fragmented than human sleep during a 24-hour period, whereas human sleep is monophasic and of long duration.
| SPECIES | TOTAL SLEEP TIME | REM SLEEP TIME |
|---|---|---|
| Opossum | 18 hours | 0.5 hours |
| Platypus | 14 hours | 8 hours |
| Dolphin | 10 hours | 0.2 hours |
| Guinea pig | 9.5 hours | 1 hour |
| Human | 8 hours | 2 hours |
| Sheep | 5.9 hours | 0.6 hours |
| Horse | 3 hours | 0.5 hours |
Little is known concerning what a guinea pig dreams — if it dreams. And little is known about why sleep is necessary for mammals — which greatly increases potential vulnerability to predators.
One of the most prominent theories about the function of REM sleep is that it facilitates the assimilation of new memories and experiences. Animal studies have indicated an increase in REM sleep after training, and have also indicated deceased memory when REM sleep is deprived.
Sleep is now being studied in fruit flies and nematodes, despite the fact that these organisms do not display EEG patterns. They do, however, exhibit periods of dormancy, and show signs of sleep deprivation if not allowed their periods of dormancy [SCIENCE; Youngsteadt,E; 321:334-337 (2008)]. A gene mutation in mammals which causes less need for sleep is associated with a greater need for REM sleep [SCIENCE; He,Y; 325:866-870 (2009)].
Over the last century electric lights, all-night groceries and increasingly stimulating activities/entertainment have contributed to reducing the amount of time people spend sleeping. Average sleep per night in the United States may have declined as much as two hours since the year 1900. Driven by a desire to accomplish more or to experience more, people often discount the value of sleep by postponing going to bed to check e-mail, do more tasks or enjoy extra entertainment. Adhering to a regular bedtime and avoiding stimulating activities before retiring is often a means of improving sleep.
Most people use coffee, tea or soda-pop to maintain wakefulness through the day. The half-life of caffeine (the time it takes for caffeine concentrations in the bloodstream become half) can vary between 3 to 7 hours (depending on the person), which means that significant amounts of caffeine can remain in the bloodstream at night due to beverages consumed in the early afternoon, or even in the morning.
Prescription medications to facilitate sleeping have improved considerably, but are still suffering from the stigma associated with earlier medications. Barbiturate sleeping pills can be addicting and can lead to death if an overdose is given. Like barbiturates alcohol can make it easier to fall asleep, but not result in restful sleep. The shift from barbiturates to benzodiazepines (such as Valium) in the 1970s eliminated the potential for fatal overdose, but not the potential for addiction. The newest hypnotics, imidazopyridines (such as Ambien) are not regarded as having addiction potential, and are safer than non-prescription "sleep-aids", such as anti-histamines. (The antihistamine pyrilamine maleate is the active ingredient for Nytol, Sleep-Eze and Sominex.) A CONSUMER REPORTS survey reported that 15% of respondents had taken a prescription drug for sleep in the preceeding month — nearly half of which were anti-depressant or anti-anxiety medications [CONSUMER REPORTS; 73(9):12-15 (2008)].
Melatonin and L−tryptophan are widely used to induce sleep, but some physicians are concerned about quality control of non-prescription pills and the absence of rigorous testing for possible harmful side effects. (The potential for melatonin to interfere with growth & development in teenagers was mentioned earlier.) As little as one or two grams of L−tryptophan is effective in decreasing sleep latency time [PSYCHOPHARMACOLOGY; Schneider-Helmert,D; 89(1):1-7 (1986) and PHARMACOPSYCHIATRY; Demisch,K; 20(6):242-244 (1987)]. L−tryptophan either improves or has no effect on other sleep parameters, with the exception of a suppressive effect on REM sleep [EUROPEAN NEUROLOGY; Korner,E; 25(Suppl 2):75-81 (1986)]. Studies with 2 mg (2 milligrams) of prolonged-release melatonin in insomnia patients over age 55 showed significantly reduced sleep onset latency (9 minutes) as well as improved sleep quality and morning alertness [JOURNAL OF SLEEP RESEARCH; Lemoine,P; 16(4):372-380 (2007) and INTERNATIONAL CLINICAL PSYCHOPHARMACOLOGY; Luthringer,R; 24(5):239-249 (2009)]. Three grams of glycine daily has been shown shown to improve sleep quality in young (average age 31) female Japanese adults [SLEEP AND BIOLOGICAL RHYTHM; Inagawa,K; 4:75-77 (2006)]
People who exercise sleep more deeply and have less difficulty falling asleep — as long as they don't exercise immediately before bedtime. High carbohydrate foods induce sleep much more readily than high protein foods.
Afternoon naps (siestas) are a common means of alertness restoration in South America, China, India and the Mediterranean, but have a bad reputation as being slothful or an aging disability in most Western countries. "Westernization" of world economies is reducing the prevalence of napping — and increasing the use of caffeine. The combined effects of being awake from morning and the afternoon dip in circadian rhythm alertness have caused some researchers to believe that naps are a "biological need". Thomas Edison and Winston Churchill were famous for their use of afternoon naps as a means of extending their productive working hours.
Napping is more frequent among people who are older and in poor health. A study of mostly middle-aged American volunteers found that over a ten-day period 29% did not nap, and the median number of nap-days was 2.5 days and the median nap length was about 35 minutes [JOURNAL OF CLINICAL SLEEP MEDICINE; Owens,JF; 6(4):330-335 (2010)]. Sleep-deprived subjects show benefits for alertness from naps as short as ten minutes, but show no benefit from naps lasting only 90 seconds [JOURNAL OF SLEEP RESEARCH; Tietzel,AJ; 11(3):213-218 (2002)].
Dr. Dement recommends immediate "emergency naps" for people having trouble keeping their eyes open while driving. For people who can tolerate caffeine Dement recommends drinking coffee before the nap. Caffeine from coffee takes about 15 to 30 minutes for the full effect to be felt, allowing for the benefits of both a 15 minute nap and of the caffeine, without the danger of a longer sleep.
Sleep is said to be regulated by a circadian component and a homeostatic component. The homeostatic component causes an increase in sleep need that varies directly with duration of wakefulness and is reduced by slow wave sleep (corresponding to EEG delta waves). The frontal association area of the brain is the most active brain area during wakefulness, and shows the strongest delta wave recovery in response to sleep deprivation [CEREBRAL CORTEX; Ferrara,M; 12(7):737-748 (2002)].
The K−complexes seem in slow wave sleep are known to arise from neurons in the cerebral cortex [SLEEP MEDICINE REVIEWS; Amzica,F; 6(2):139-149 (2002)]. Sleep spindles arise from the reticular nucleus of the thalamus and the projections of the reticular nucleus into the cerebral cortex (primarily during the lighter stages of sleep) [SLEEP MEDICINE REVIEW; De Gennaro,L; 7(5):423-440 (2003)]. Sleep spindle activity is important for the integration of new memories into existing knowledge [JOURNAL OF NEUROSCIENCE; Tamminen,J; 30(43):14356-14360 (2010)]. K−complexes & sleep spindles decline significantly in the elderly [CLINICAL NEUROPHYSIOLOGY; Crowley,K; 113(10):1615-1622 (2002)].
A homeostatic indicator of increasing sleep deprivation during extended quiet waking is the amplitude of theta waves (believed to arise independently from the hippocampus & neocortex of humans) — providing a quantitative measure of sleep propensity when awake and predicted sleep intensity when asleep [BRAIN RESEARCH; Vyazovskiy,VV; 1050(1-2):64-71 (2005)].
Three distinct components of learning & memory are described: (1) acquisition (2) consolidation and (3) retrieval. Sleep is believed to play a crucial role in consolidation, during which new memories are integrated into existing long-term memories. A distinction is also made between declarative & procedural memory. Declarative memories are memories of facts, such as the name of the capital of Brazil. Declarative memories can often be remembered as a result of a single learning event. Procedural memories (such as knowing how to touch type, tie a shoe or ride a bicycle) often require repeated trials for learning. It is characteristic of procedural learning that delays & sleep following a training lead to performance gains.
Encoding and short-term retrieval of declarative memories is heavily dependent upon the hippocampus, but with consolidation these memories become stored & retrieved in the cerebral cortex. Reactivations of newly encoded declarative memories in the hippocampus leading to consolidation occur during slow wave sleep (SWS,NREM sleep), in association with sleep spindle [THE NEUROSCIENTIST; Born,J; 12(5):410-424 (2006)]. A learning task associated with activation of Brodmann areas 40 & 7 of the cerebral cortex was shown to correlate with slow wave activity in those areas during sleep — and improved performance of the task after sleep [NATURE; Huber,R; 430:78-81 (2004)].
Procedural memories, by contrast, are consolidated during REM sleep. Higher levels of procedural learning are associated with a higher intensity of REM sleep [LEARNING & MEMORY; Smith,CT; 11(6):714-719 (2004)]. REM sleep is also associated with consolidation of "emotional memories" and learning of complex games. In REM sleep there is less flow of information from the hippocampus to the neocortex, and much greater activity in the limbic system (amygdala and the anterior cingulate cortex). Reduced activity of the decision-making areas of the prefrontal cortex during REM sleep are postulated to reduce attention to the bizzare incongruities of dreams [SCIENCE; Stickgold,R; 294:1052-1057 (2001)]. Much about consolidation of memory during sleep is still unresolved.
The control of sleep & alertness involves a bewildering array of chemicals & neural structures. Benzodiazepines (like Valium®) and barbiturates (like phenobarbital) induce sleep by potentiating GABA — the primary inhibitory neurotransmitter — all over the brain (increasing the amount of time spent in stage II non-REM sleep). The tubermammillary nucleus of the posterior lateral hypothalamus tonically releases histamine throughout the cortex as a wakefulness-promoting neuromodulator (which is why anti-histamines can cause drowsiness). Amphetamines, the most potent promoters of wakefulness, increase dopamine availability [THE JOURNAL OF NEUROSCIENCE; Wisor,JP; 21(5):1787-1794 (2001)]. Benzodiazepines (eg, valium) increase Stage 2 sleep, while decreasing the other Stages, including Slow Wave Sleep and REM sleep [JOURNAL OF SLEEP RESEARCH; Perlis,L; 6(3):179-188 (1997)]. Melatonin from the pineal gland can influence the circadian sleep-waking cycle through the suprachiasmatic nucleus.
A neural structure that is central to wakefulness is the reticular activating system in the brainstem — notably the raphe nuclei (associated with serotonin), the locus coeruleus (projecting norepinephrine) and the peribrachial nuclei (projecting acetylcholine) — which activates the higher brain centers. Lesions of the raphe nuclei result in insomnia. All three neuromodulators are actively projecting in the waking state, and all three are less active during non-REM sleep (SWS). Acetylcholine from the brainstem activates both the histamine-producing tubermammillary nucleus in the hypothalamus and the basal nucleus of the forebrain, which itself sends acetylcholine to the cerebral corex as an arousal-promoting neuromodulator. The basal nucleus is also activated by norepinephrine from the locus coeruleus. Both serotonin & noradrenaline levels drop to near zero in REM sleep, but acetylcholine levels are as high or higher in REM than in waking [SCIENCE; Maguet,P; 294:1048-1051 (2001)]. Acetylcholine enhances cortical plasticity. Serotonin, on the other hand, can inhibit REM sleep [SLEEP; Datta,S; 26(5):513-520 (2003)]. Cortisol also inhibits REM sleep, and the decline of REM sleep with senescence is primarily due to increased plasma cortisol [THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM; Vgontias,AN; 88(5):2087-2095 (2003)].
Adenosine acts like a neurotransmitter in the brain, but is not released from synapses. Instead, adenosine is released by both neurons and glial cells as a result of the breakdown of the energy-supplying ATP (Adenosine TriPhosphate) molecules. Thus, a rise in brain adenosine is associated with a depletion of energy in the brain cells. Appropriately, the action of adenosine on brain adenosine receptors is to induce sleepiness (so that resting can replenish ATP) [THE JOURNAL OF NEUROSCIENCE; Thakkar,MM; 23(10):4278-4287 (2003)]. Caffeine blocks the action of adenosine receptors. Individuals who are more sensitive to the effects of caffeine are also more sensitive to the effects of sleep deprivation [THE JOURNAL OF NEUROSCIENCE; Refey,JV; 26(41):10472-10479 (2006)].